Almost everything you need to know about masking in audiology, including the reasoning behind masking in occupational health.
Many clinicians break out in a cold sweat when it comes to masking in audiology. “Am I doing this correctly? Is it effective?” Take a deep breath and read on.
First, we must understand the science and reasoning behind masking in occupational health. We also have to cover some of the related concepts, such as interaural attenuation (IA) and the occlusion effect (OE). You may already know these terms, but we will shed some light on how they all work together.
What Is ‘Masking’ in Occupational Health?
When being tested, it is possible for the non-test ear to hear a tone presented in the test ear. We call this crossover.
It happens when a signal conducted by air is strong enough to cause vibration of the skull. Sound is transmitted through bone conduction and allows the patient to hear the tone in the non-test ear. Because the skull is fused, these vibrations activate fluid motion within the cochleas of both ears.
Tones produced by insert earphones, such as those found in Kuduwave audiometers, can only cause vibrations in the deeper part of the ear canal. Therefore, tones played through inserts need greater intensity to generate crossover. Supra-aural or circumaural earphones (that make contact with the head) can more easily cause vibration. This can affect testing and subsequent hearing aid fitment.
In short, supra- and circumaural earphones generate crossover at a lower intensity than inserts. If crossover becomes present, the clinician would have to isolate the test ear from the non-test ear. This is performed through masking.
In audiology, masking means playing white noise in the non-test ear, to prevent it from hearing the tones that cross over from the test ear.
In audiology, masking means playing white noise in the non-test ear, to prevent it from hearing the tones that cross over from the test ear. It helps to obtain the true threshold of the test ear and ensures that the non-test ear is not ‘assisting’.
Interaural attenuation
The level of masking noise required depends on the volume of the signal that might cross over.
To a certain degree, interaural attenuation (IA) reduces crossover. Interaural attenuation refers to the volume of sound intensity attenuated (reduced) when crossing from the test ear to the non-test ear. Known average interaural attenuation values are available for insert earphones, as well as for supra- and circumaural earphones.
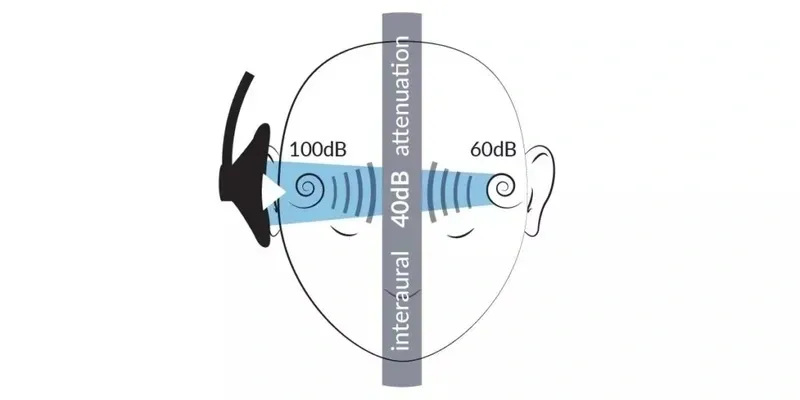
Study results from Chaiklin (1967), Killion, Wilber & Gundmundson (1985) and Sklare & Denenberg (1987) on supra- or circumaural earphones, found average interaural attenuation values across all frequencies for air conduction to be around 60 dB. In testing, a more conservative interaural attenuation of 40 dB is used.

For inserts, results from Killion et al. (1985), Konig (1962) and Sklare & Denenberg (1987) found average interaural attenuation values of around 80 dB, with minimum levels of 70 dB. Therefore, a clinician can use 70 dB during masking. However, most clinicians use a much more conservative 60 dB for inserts.
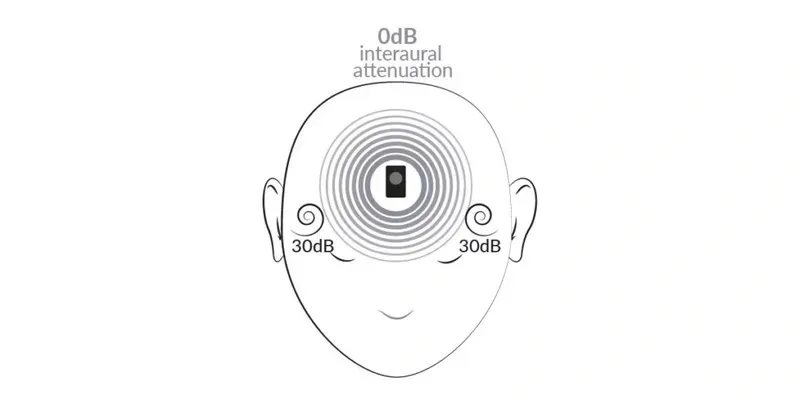
Adult skulls are fused at the cranial sutures. If you vibrate any part of the head bone (i.e. Mastoid), equal vibrations will transmit to the the entire head bone and both cochleas. This means that there is almost no (>10dB) interaural attenuation in bone conduction testing. The most conservative assumption is that there is no interaural attenuation. This assumes that the ‘entire’ intensity will go to the non-test ear too.
In audiometric testing, most patients will not experience crossover at the levels mentioned above. Yet, one cannot assume the patient’s attenuation value, without calculating each patient’s individual interaural attenuation values. Therefore, we use masking based on the generally validated interaural attenuation values when crossover may occur.
The occlusion effect
The occlusion effect is the enhancement of bone-conducted sound waves caused by blocked or occluded ear canals. The occlusion effect occurs when the occluded ear canal traps the bone-conducted signal energy. This causes an increase in sound pressure levels delivered to the tympanic membrane and inner ear. This can improve bone-conducted thresholds and deliver false test results.
Therefore, bone-conduction masking requires a correction factor for the occlusion effect (OE) caused by the earphone in the non-test ear being masked. The correction factor increases the normal masking level to offset the added sound pressure transmitted to the cochlea, and applies to 250-, 500- and 1 000-Hz frequencies.
Occlusion-effect masking
Occlusion-effect masking values will depend on what is occluding the ears (insert or supra-aural earphones). Various studies in the field of occupational health recommend different occlusion-effect correction values. When using inserts, Dean & Martin (2000) recommend correctional values of 9 dB for 250 Hz, 7 dB for 500 Hz, and 0 dB for 1000 Hz. When using deep-insert earphones, the occlusion-effect values are low.
The deeper the earphone is inserted in the ear canal, the smaller the remaining resonating area becomes. This is why a deep insert is crucial to success when using the above-mentioned OE values.
When using supra-aural earphones, Goldstein & Newman (1994) recommend correctional values of 15 dB for both 250 Hz and 500 Hz, and 10 dB at 1 000 Hz. Studies show there is very little occlusion-effect variation between forehead and mastoid bone-conduction placement, but that it is significantly reduced when using insert earphones.
Below is a method for calculating each patient’s specific occlusion-effect values; whether using insert or supra-aural earphones. Warning: This takes up valuable clinical time.
Calculating occlusion-effect values for masking in audiometric testing:
Step 1: Place the bone vibrator on the preferred site (mastoid or forehead).
Step 2: Measure the patient’s bone-conduction thresholds at 250, 500 and 1 000 Hz, without occluding the ears.
Step 3: Measure the patient’s bone-conduction thresholds with occluded ears (or occlude the non-test ear) using insert or supra-aural earphones.
Step 4: Subtract results of bone-conduction occluded thresholds from the bone-conduction unoccluded thresholds. This is the patient’s occlusion-effect value.
Step 5: Now add the occlusion-effect value of 250, 500 and 1 000 Hz to the total masking value of the noise in the non-test ear.
Masking for Air Conduction vs Bone Conduction
Air-conduction testing
In air-conduction (AC) testing, the main concern is that high-volume, pure-tone, air-conduction sound may generate bone-vibration sound and be audible in the non-test ear. Each patient’s physiology is different, so not everyone will experience crossover at the same intensity level.
When to mask
A general rule is to compare the air conduction thresholds of the test ear with the bone-conduction thresholds of the non-test ear. If the difference between the non-test ear bone-conduction and test ear air-conduction thresholds is 40 dB or more, when using supra-aural earphones, then you should mask. For insert earphones, the difference should be 60 dB or more.
The formula for determining whether masking is needed:
Mask if: AC (test ear) – IA (40 dB or 60 dB) ≥ BC (non-test ear).
Generally speaking, audiologists determine when to mask by comparing the air-conduction thresholds of the test ear and the non-test ear. This is because many audiologists often obtain air-conduction thresholds prior to measuring and obtaining bone-conduction thresholds. A preliminary decision can be made about the need to mask by comparing the air-conduction of the two ears (Katz, 2014).
Remember that crossover hearing occurs primarily through the mechanism of bone conduction. As a result, it may be necessary to re-evaluate unmasked bone-conduction thresholds in order to determine the need for masking the non-test ear during air-conduction testing.
From a clinical perspective, the need to mask by comparing air-conduction thresholds in the patient’s ears may not be immediately evident. However, once unmasked bone-conduction thresholds are obtained, contralateral masking may be required, based on the ‘when-to-mask’ formula above.
When using inserts for air-conduction testing, it is less likely that masking will be needed.
At what level should I mask?
To mask the non-test ear, add 10 dB HL to the air-conduction threshold in the non-test ear (air conduction non-test ear + 10 dB HL). For effective masking, start at this level.
Bone-conduction testing
By this time, you may have realised the audiometric tester should always mask if the interaural attenuation for bone conduction is ~0 dB. Most audiologists agree and will always mask during bone-conduction testing. Even ANSI (2004) assumes masking was or is always used during bone-conduction testing.
The British Society of Audiology (2012) further advocates for masking during bone conduction by stating that ‘without masking [during bone-conduction testing], it is not possible to determine which ear is responding to bone conduction… When testing without masking, thresholds may appear more acute by about 5 dB due to binaural stimulation.’
When masking the non-test ear, the listening task becomes slightly difficult and results in elevated threshold of the test ear compared to what would have occurred without masking the non-test ear.
Known as central masking – this is a side effect of non-test ear masking noise being near-threshold-levels which often creates a 5 dB threshold elevation. If you don’t mask, the threshold will likely be 5 dB better and present minor air-bone gaps.
When should I mask for bone conduction?
In short, always. Since interaural attenuation during bone conduction is ~0 dB, the intensity at both cochleas is equal. The more responsive cochlea will detect the sound. There is no need for masking if bone-conduction test results rule out a conductive component (i.e. no air-bone gap). If there are air-bone gaps, we should then mask to determine if they are ‘real’ air-bone gaps and whether they are unilateral or bilateral.
If there is an air-bone gap of more than 10 dB in the test ear, masking is needed.
The formula for deciding whether you should mask or not:
Mask if the air-bone gap in the test ear ≥ 10 dB.
How much masking is needed?
To mask the non-test ear for for bone-conduction testing, add 10 dB HL to the air-conduction threshold in the non-test ear and add the occlusion effect (air conduction non-test ear + 10 dB HL + occlusion effect). That is the level you can start masking at.
Masking strategy
Several masking techniques or methods exist in occupational health. The most popular is the plateau method. Using this method, the above formulas for bone conduction and air conduction determine the starting level for masking. The starting decibel level for the test ear will be the unmasked test ear threshold you have recorded.
Step 1: Determine the starting levels.
Step 2: Present the masking noise into the non-test ear, while simultaneously presenting the unmasked threshold (signal) into the test ear.
Step 3: Increase the masking noise in the non-test ear by increments of 3 by 5 dB steps (+5dB, +5dB, +5dB).
Step 4: If the tone is still heard after increasing the masking level three times, then that is your threshold.
Step 5: Obtain three consecutive responses to three increments.
The masking dilemma
A common issue with masking in audiometric testing is locating the masking plateau. This is called the masking dilemma and it occurs when there is moderate to severe bilateral conductive hearing loss. In this case, masking noise intensity presented in the non-test ear crosses over to the test ear and elevates the thresholds. This means the clinician would keep masking, without reaching the plateau.
A simple workaround for the masking dilemma in occupational health is using insert earphones. Inserts provide superior inter-aural attenuation to their counterparts and reduce the need to mask in the first place.
If you still cannot get a true threshold, as a result of the masking dilemma, it is best to record the unmasked threshold on the audiogram as ‘could not mask’.
Kuduwave Does Simple and Efficient Masking
The Kuduwave masking strategy saves the clinician valuable time in determining accurate masked thresholds. It can mask manually or automatically for bone conduction, with the occlusion effect automatically accounted for.
Air-conduction masking works manually, allowing for any masking strategy or procedure that you believe yields the best results. (We recommend the plateau-masking method, described above.)
This is especially useful in cases of tele-audiology as it’s crucial to be sure you can trust your results when conducting remote tests.
The combination of insert earphones, simplicity and quick masking is just another feature that sets the Kuduwave apart in occupational health. It also provides improved patient comfort, infection control, ambient noise attenuation, and much more.
To experience the Kuduwave’s special features, book a free product demo with your distributor.
JOIN OUR COMMUNITY
Keep up to date with the latest news at GeoAxon
[contact-form-7 id=”67a1462″ title=”Contact form 1″]